Gain new perspectives for faster progress directly to your inbox.

Recent clinical trials show that recreational psychedelics like LSD (Lysergic acid diethylamide), MDMA (3,4-Methylenedioxymethamphetamine), sometimes known as ‘Molly’), and Psilocybin (sometimes known as ‘Shrooms’) when properly controlled for dosing and administration are having positive outcomes. With an increasingly global problem and no new classes of antidepressants in the last 30 years, could psychedelics be another tool in the fight against depression and PTSD?
Why does mental health matter? A growing problem and opportunity
A healthy population is the cornerstone of a thriving and prosperous economy. But according to the World Health Organization (WHO), over 280 million people suffer from depression, and an estimated 284 million people have suffered from post-traumatic stress disorder (PTSD) across the world. We know that mental illness negatively impacts people’s ability to work, and can significantly limit their participation in the labor market. In fact, depression is the leading cause of disability worldwide and with remission rates for PTSD ranging from 20-30%, there is a growing population that is seeking care.
Subsequently, there is a case to be made for the urgency of tackling a growing mental health crisis. The rates of mental illness among adolescents and young adults have increased significantly over the last decade, and the COVID pandemic has accelerated this impact. Despite this, there has not been a significant breakthrough in research or a revolution in the corresponding treatments to alleviate the issue. In fact, many big pharmaceutical companies backed away from research and development in mental illness drugs and narrowed their investment in neuroscience research programs due to high risks and high failure rates in clinical trials.
The status quo: Treatment resistance with current anti-depressants
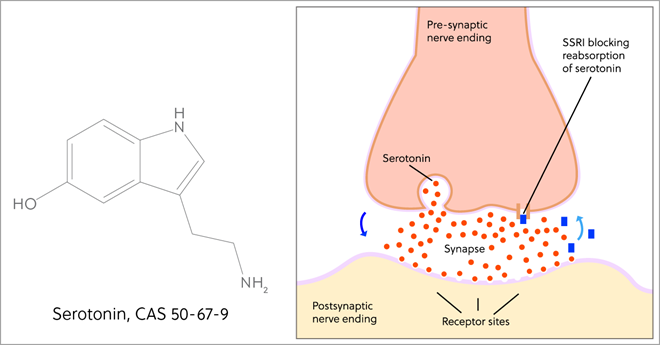
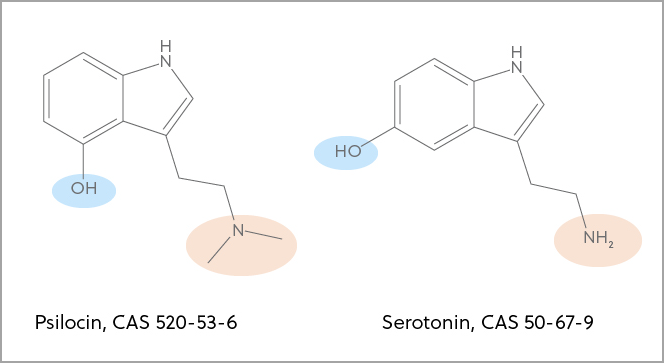
It has been over 30 years without a novel class of anti-depression medications. Selective serotonin reuptake inhibitors (SSRIs), such as Prozac, have been the major class of anti-depression medication for several decades. Serotonin is a key hormone that activates the serotonin receptors in certain regions of the brain to stabilize our mood, feelings, and happiness (Figure 1).
The SSRI drugs work by inhibiting the reuptake process of serotonin (5-HT) at the neuronal synapses in a way to increase the serotonin level at the synapses (Figure 1). However, many patients have developed treatment resistance to these drugs after many years of prescription, which is resulting in a significant demand to find new ways of treatment. Could psychedelics be one of those ways?
Promising results in early clinical trials
Since 1990, there has been increased research interest in psychedelic drugs due to the technological advancement in neuroimaging, allowing researchers to link these drugs with an actual materialized outcome in an experimental setting. These drugs are a class of hallucinogenic substances, that exert their neurological effect by binding to some of the neurotransmitter receptors (receptors sensing chemical signals between neurons). After ingestion, they produce changes in people’s perception, mood, and cognitive process and may take one to a mental trip away from reality, called a “psychedelic trip.” These drugs are organic chemical compounds, either synthesized or extracted from natural sources.
Given the increasing awareness of mental health problems and the fact that the current situation of inadequate available treatments, psychedelic drugs are finding their renewed value as a tool for treating a variety of mental illnesses. Here, we take a look at three psychedelic drugs which currently in the late stage of clinical trials:
- Psilocybin (shrooms) for the treatment of drug-resistant depression in phase 2 trials
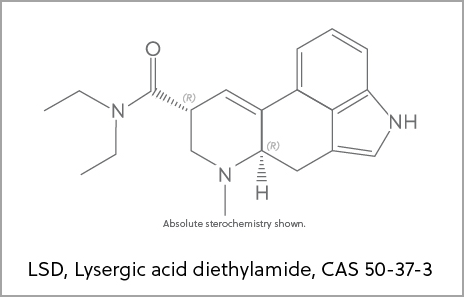
- Lysergic acid diethylamide (LSD) for the treatment of major depressive disorder in phase 2 trials
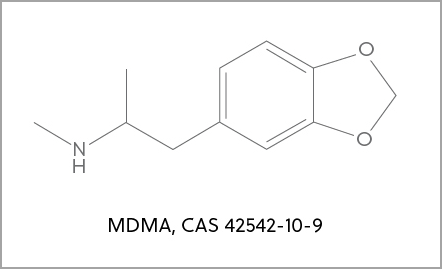
- 3,4-Methylenedioxymethamphetamine (MDMA) a key ingredient in the drug commonly known as ecstasy or molly, for the treatment of PTSD patients in phase 3 trials.
Mushrooming potential for psilocybin
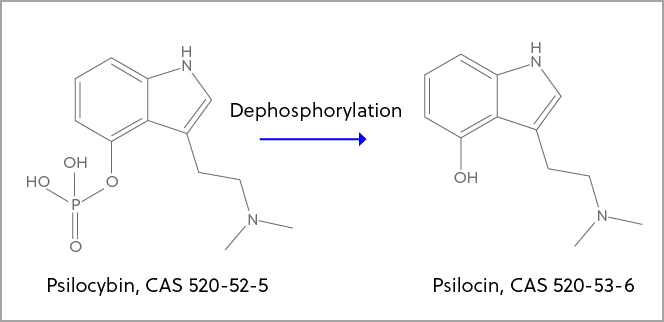
Once ingested, psilocybin is turned into the active drug form of psilocin (Figure 2) and its chemical structure is very similar to serotonin, allowing it to function as a serotonin receptor agonist. The only differences in the structures are the positions of hydroxyl and methyl groups (Figure 3). Over a few hours after ingestion, psilocybin produces profound changes in consciousness with visual and auditory hallucinations.
From a randomized clinical trial, psilocybin-assisted therapy was found to be efficacious in producing large, rapid, and sustained antidepressant effects in patients with major depressive disorder. Currently, psilocybin is in phase 2 clinical trial for major depressive disorder. In addition, several pilot studies of psilocybin-assisted psychotherapy also have shown positive benefits in treating both alcohol and nicotine addiction.
Early outcomes showed of LSD
Like psilocybin, LSD can also be found and extracted from mushrooms. However, it was first chemically synthesized by Switzerland scientist Dr. Albert Hofmann in 1938. The psychological effect of LSD was heavily investigated during the years from 1950-1970. Many publications during that period showed positive behavioral and personality changes in patients with various psychiatric disorders. It was also observed that LSD together with suitable accompaniment during its administration, could reduce pain, anxiety, and depression in patients with advanced cancer.
Like psilocybin, LSD mainly works as a serotonin receptor agonist due to its structural similarity with serotonin (Figure 4). However, it is still poorly understood in the mechanisms of interactions between the receptor activation and the resulting impairment in cognition and induction of hallucinations. Nevertheless, the benefit of LSD in treating various mental illnesses is currently being investigated in several pilot clinical studies. More promisingly, LSD with different doses is being tested in a phase 2 trial for major depressive disorder.
MDMA moves beyond raves
MDMA is a synthetic psychedelic drug (Figure 5). It has been popularly used at nightclubs as a party drug. MDMA primarily acts as an indirect serotonergic agonist to increase the amount of serotonin released into the synapse. It also acts on serotonin storage vesicles and serotonin transporters to increase the amount of serotonin ready to be released and to promote its release. This process can lead to significant increases in serotonin available in the synapse. MDMA has been shown to enhance fear memory extinction, modulate fear memory reconsolidation, and bolster social behavior in animal models.
More interestingly, recent work done by a research team at Johns Hopkins revealed its therapeutic value and potential mechanism in treating PTSD patients. The team discovered that MDMA was shown to reopen the otherwise closed critical periods for neuronal circuits formation in disease states, allowing the reformation of the neuronal circuits when environmental stress is no longer present. MDMA is currently in phase 3 trial and its phase 2 trials have shown promising safety and efficacy findings in treating PTSD patients.
Progress, but more work required
While progress has been made, there are still some roadblocks to using psychedelics in the treatment of mental health disorders. First, outside of Oregon, many of these substances are schedule 1 controlled substances and are illegal. Secondly, the potential for abuse, neglect, and misuse of highly controlled substances is high with both patients and providers. Finally, there are physical risks as well. A few patients occasionally may experience a “bad trip,” described as an acute state of anxiety and confusion, or they experience a moderate increase in blood pressure and heart rate.
Although psychedelic drugs do not cause dependency or withdrawal issues as opioids or cannabis substances do, long-term use or frequent use may lead to tolerance. It is advised that psychedelic drugs should be administrated to the patients in a controlled and supervised environment.
Mental health is not a simple black and white status; it is complex—spectral and continuous. At the positive end, mentally thriving and fulfilling; in the middle, coping and surviving; and at the negative end, daily functions disrupted by illness. Treatment options should also be addressed on a continuum in a highly collaborative environment with the patient and their healthcare providers. This may range from cognitive behavioral therapy to known drugs or procedures, to more experimental approaches depending on the doctor’s diagnosis and assessment.
As innovation continues to accelerate in this exciting therapeutic area, CAS recently partnered with April 19 Discovery, an AI-driven drug discovery company specializing in psychedelics. This machine learning collaboration has accelerated lead compound development for April 19 Discovery through the CAS Content CollectionTM and customized services. Learn more in the press release.